A baby received an exchange blood transfusion. This is a specialist and complex procedure with associated risks (and is now infrequently performed in most neonatal units). During the exchange transfusion procedure, the baby’s condition deteriorated and they had a cardiac arrest, which was due to hypovolaemia as the incorrect infusion line had been used. The baby was later diagnosed with severe brain injury, meeting the criteria for MNSI investigation.
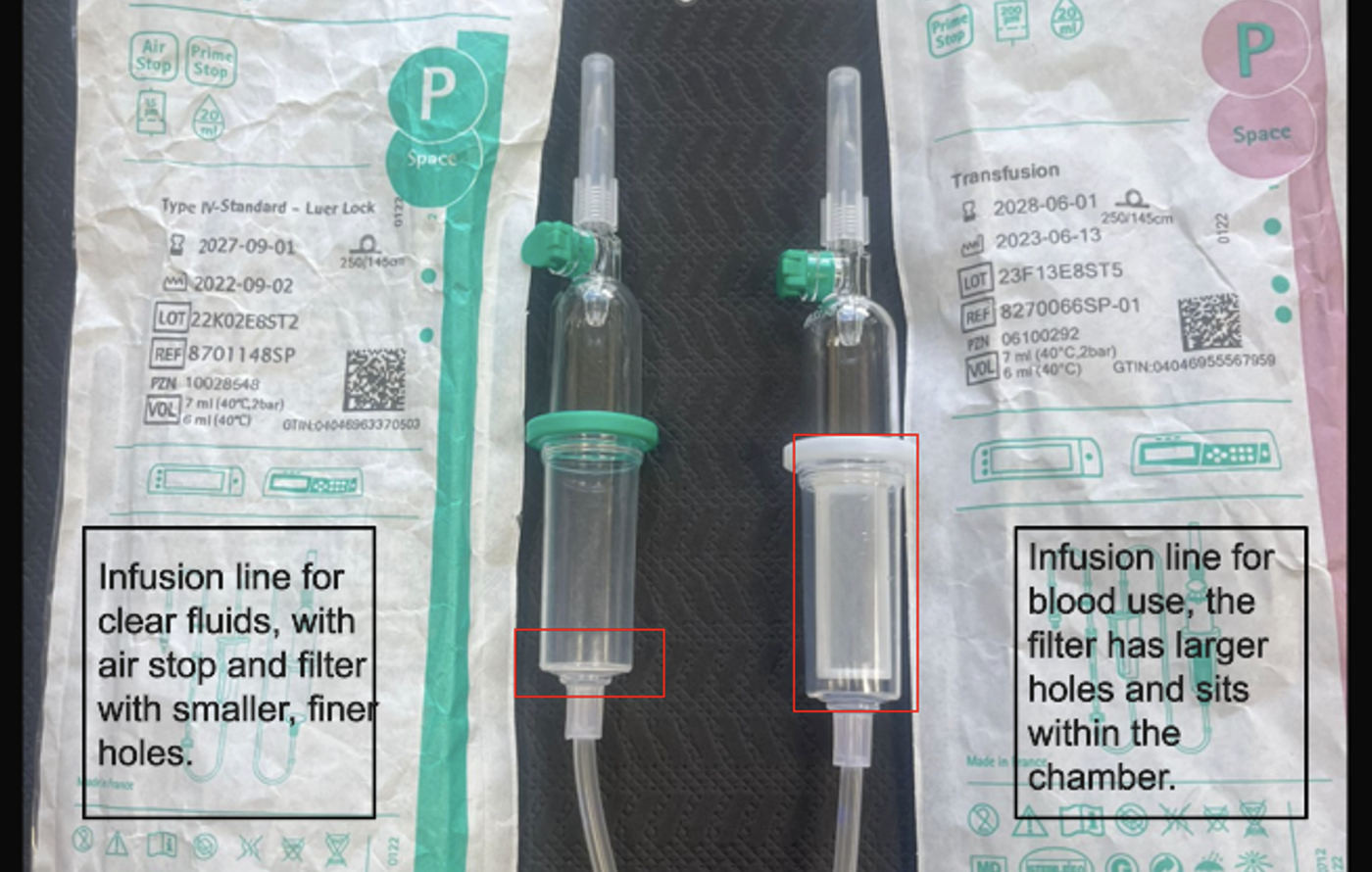
The procedure for transfusing donor blood involved the use of a multi-function, volumetric pump and a specific infusion line for use with blood. Pre-made procedure packs contained the incorrect infusion line for the administration of blood. The packs contained an infusion line for clear fluids, which has a much finer filter, with smaller holes, this means that red blood cells cannot effectively pass through the filter. For the volumetric pump used, the packaging of the different infusion lines differs in colour; the differences are less obvious without the packaging.[1] It was not recognised that the incorrect infusion line was being used.
Priming the infusion line took much longer than expected; visually blood was seen moving through the line which gave reassurance that the equipment was working as intended. During the procedure the volumetric infusion pump showed that the expected volume had been infused, which meant staff were not alerted that the baby was not receiving sufficient blood until after their condition deteriorated.
- Does your local process ensure a repeat bilirubin is measured before starting the exchange transfusion to ensure that it is still required?
- Are all staff aware that infusion lines differ and know about the different filter characteristics?
- How are staff supported to recognise different infusion lines?
- Where equipment is collected into ‘packs’ for a procedure, how does the trust ensure the correct equipment is included?
- How do staff, of all levels of seniority, recognise and seek help when events are not progressing as expected? For example, how long the infusion line should take to prime and when should this trigger a review of the equipment being used?
- Does local simulation training include the use of the incorrect infusion line with expired blood, to demonstrate the impact of this on the procedure?
- How does the local system of recording and overseeing a baby’s observations support staff to recognise changes in their condition during the exchange transfusion?
- Does your local process for exchange transfusion include a role, focussed on oversight of the transfusion, to help recognise and respond to any deterioration, including stopping the procedure?
[1] This equipment issue has been reported to the MHRA via the Yellow Card scheme, in accordance with regulatory requirements for medical device safety.